Scientists recently made substantial progress in developing Natural Killer (NK) cells as an off-the-shelf immunotherapy for oncology applications. NK cells play a critical role in tumor surveillance, which underpins much of the research of NK cells as a cancer treatment.
Specifically, the NK-92 cells have been successfully modified to express high affinity receptors that can recognize antigens expressed on tumor cells and mediate NK cell activation.
Researchers at MD Anderson, ImmunityBio and several other institutes have conducted phase 1/2 clinical studies to establish the safety of administering NK-92 cells as allogeneic cell therapy in hematologic and solid cancers with promising results.[1]
Basics of Natural Killer Cells
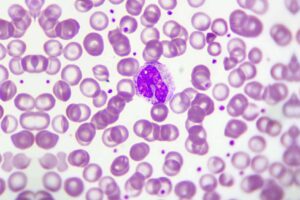
NK cells are lymphocytes that are part of the innate (nonspecific) immune system. The innate immune system is the first line of defense against infectious agents, can recognize and clear tumor cells, and interfaces with the adaptive (specific) immune system.
It has long been recognized that NK cells have crucial anti-tumor activity and, unlike T-cells of the adaptive immune system, NK cell anti-tumor function occurs without the need for prior sensitization.[2]
CAR-T cell immunotherapy represents a significant medical advancement for hematological malignancies; however, the toxicity profile has limited its wide clinical application.
The advantage of CAR-NK immunotherapy is a significantly reduced potential for neurotoxicity, cytokine release syndrome, and graft-versus-host disease due to its distinct cytokine profile.[3] The safer CAR-NK platform is not limited to the requirement to develop for an individual patient, making it a promising resource for off-the-shelf clinical application.
Leveraging NK Cells as an Off-the-shelf Immunotherapy
The potential to develop NK-cell immunotherapies is bolstered by the diversity of NK cell sources including hematopoietic stem cells, umbilical cord blood, peripheral blood, and immortalized NK cell lines.
One cell line, NK-92, shows reliable cytotoxic activity against a number of tumor cell types. The strong anti-tumor activity is attributed, in part, to the expression of high levels of granzyme B and perforin.[4]
NK-92 cells are considered easy to expand, another feature that makes NK-92 cells useful for the development of off-the-shelf immunotherapies.
Another salient feature of NK-92 cells is their ability to target a wide range of tumor antigens, and they have been found to exhibit cytotoxic activity in vitro against malignant hematologic cells.
Studies conducted in severe combined immunodeficient mice demonstrate anti-tumor activity of NK-92 cells in T acute lymphoblastic leukemia, acute myelogenous leukemia, myeloma, and melanoma. Meanwhile, no NK-92 tumorigenicity has been reported in this mice model.[5]
Given the in vitro and pre-clinical data for NK-92 cells, studies addressing the safety and efficacy of CAR-engineered NK-92 cells have been launched over the past two years.

Ongoing Studies
Early CAR NK-92 cell engineering targeted ErbB2, and these cells showed cytotoxicity in vitro against ErbB2-expressing cancer cells, including breast, ovarian, glioblastoma, and squamous cell carcinoma cells.[6]
The cancer cell cytotoxicity of ErbB2-CAR-NK-92 cells was also observed against human ErbB2 fibroblasts in mice. Targeting other tumor surface antigens for various tumor types were studied and found to increase survival of mice expressing colorectal, renal, and hepatocellular carcinomas, as well as prostate cancer.
CAR-NK-92 cells targeting checkpoint molecules expressed on tumor cells have been shown to suppress lung tumor growth and increase survival in experimental mice.
There are ongoing phase 1 and 2 clinical trials with CAR-NK-92 cells for the treatment of pancreatic cancer, multiple myeloma, acute myeloid leukemia, lymphoma, glioblastoma, hepatocellular carcinoma, and colorectal cancer.
Enhancements to increase the potency of CAR-NK cells are being considered and include determining the means to increase tumor infiltration and overcoming the effects of targeted antigen loss.
Conclusion
Overall, CAR-NK technology may provide immunotherapeutic approaches against solid tumors while overcoming limitations seen with CAR-T cell therapy.
CAR-engineered NK cells are adaptable to allogenic, off-the-shelf production with a lower manufacturing cost compared to CAR-T therapies.